Reinkom Medical Instruments Co., Ltd
A World-Leading Supplier Of Medical Solutions
what is a wound protector in surgery
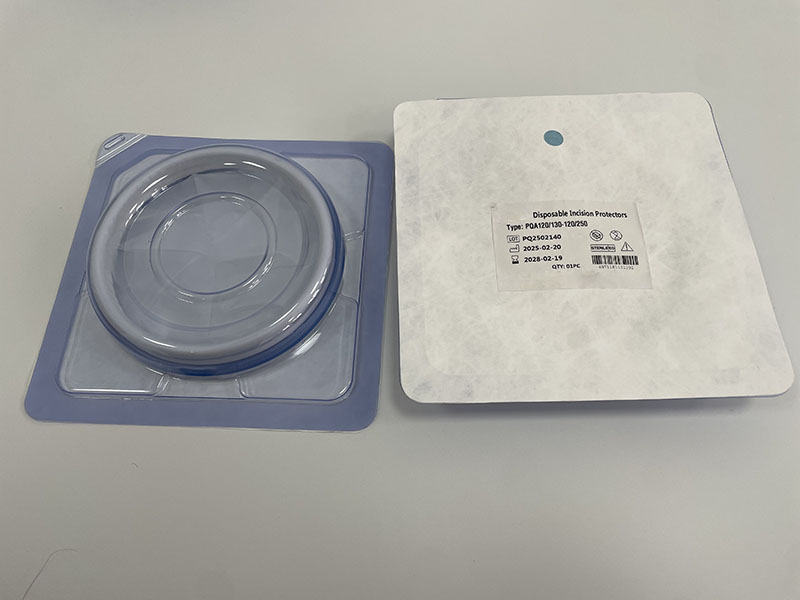
A surgical wound protector, also known as a wound edge protector or wound retractor, is a critical medical device used during surgical procedures to safeguard the incision site from contamination, minimize tissue trauma, and promote optimal healing. This article explores the definition, types, functions, clinical applications, and advancements of wound protectors in modern surgery.
Definition and Core Function
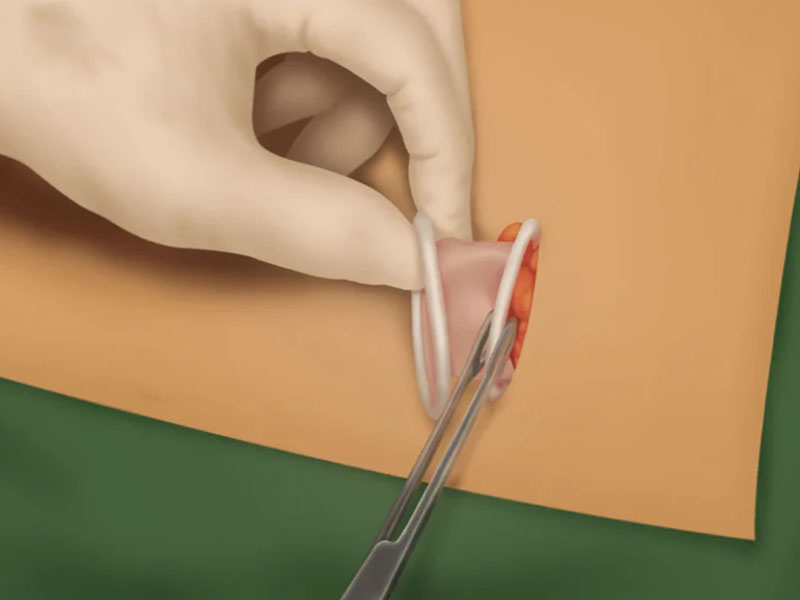
A wound protector is a sterile, flexible device designed to create a physical barrier between the surgical incision and the surrounding tissues, instruments, and body cavities. Typically composed of transparent materials like polyurethane or silicone, it features a ringed structure (single or double) that secures the protective sheath around the wound edges . Its primary role is to:
Prevent Contamination: By isolating the incision from endogenous bacteria (e.g., gastrointestinal contents during abdominal surgery) and exogenous pathogens, wound protectors significantly reduce the risk of surgical site infection (SSI) .
Minimize Tissue Trauma: The uniform distribution of tension across the incision prevents localized pressure injuries and reduces postoperative pain .
Enhance Visibility and Access: The transparent design allows surgeons to visualize the wound clearly, while the retraction mechanism widens the operative field, facilitating instrument manipulation .
Types and Design Features
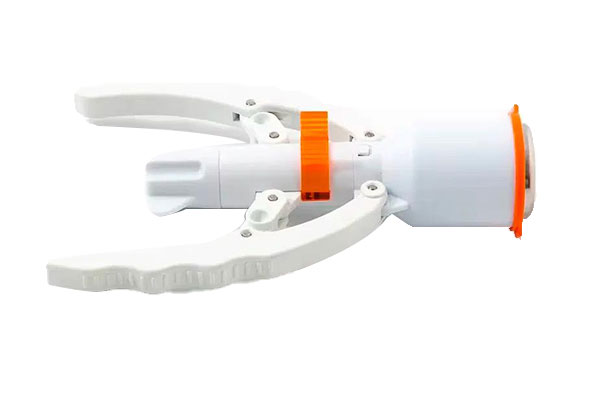
Wound protectors come in various configurations tailored to specific surgical needs:
Single-Ring vs. Double-Ring: Single-ring devices are simpler and cost-effective, suitable for smaller incisions. Double-ring protectors, with an outer stabilizing ring and an inner retracting ring, offer superior tension distribution and are preferred for larger or complex surgeries .
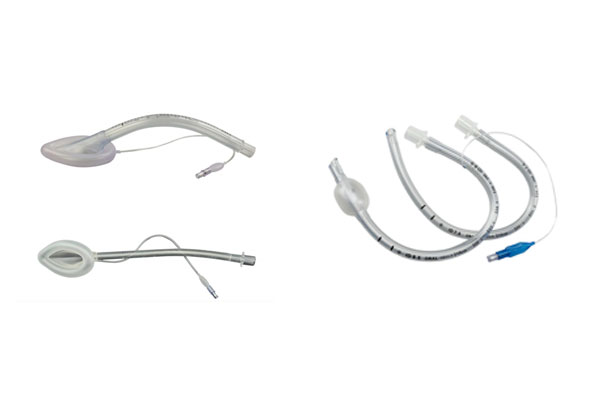
Material: Polyurethane and silicone are common materials due to their biocompatibility, flexibility, and resistance to tearing. Silicone-based protectors are often used in laparoscopic procedures for their adaptability to curved incisions .
Specialized Designs: Some protectors integrate antimicrobial coatings or drug-releasing matrices to further combat infections . For laparoscopic surgeries, self-retaining models with built-in ports allow simultaneous retraction and instrument insertion .
Clinical Applications and Efficacy
Wound protectors are widely used across surgical disciplines:
Abdominal Surgery: Meta-analyses show that wound protectors reduce SSI rates by 34-41% in clean-contaminated and contaminated procedures, particularly in gynecological and gastrointestinal surgeries . However, their efficacy in colorectal surgery remains debated, possibly due to the high bacterial load in the intestinal tract .
Laparoscopic and Minimally Invasive Surgery: These devices help maintain a sterile field during port insertion and specimen extraction, minimizing the risk of port-site infections .
Orthopedic and Thoracic Surgery: In orthopedic procedures, wound protectors protect incisions from bone debris and reduce soft tissue irritation. In thoracic surgeries, they assist in retracting ribs without causing fractures .
Advantages Over Traditional Methods
Infection Reduction: Studies report a 59-66% reduction in superficial SSIs when wound protectors are used .
Healing Promotion: By maintaining a moist wound environment and reducing mechanical stress, these devices accelerate epithelialization and collagen synthesis .
Cost Efficiency: While initial costs are higher than traditional drapes, the long-term savings from reduced infection-related complications (e.g., prolonged hospital stays, antibiotic use) justify their use .
Implementation and Best Practices
Selection Criteria: Choose the appropriate size based on incision dimensions and surgical approach. For example, laparoscopic procedures may require smaller, flexible protectors, while open surgeries need larger, rigid models .
Application:
Sterile technique is crucial to avoid contamination during placement.
The protector should be stretched evenly over the incision, ensuring the sheath covers both wound edges and retracts tissues without excessive tension .
Secure the device with adhesive strips or sutures if necessary.
Postoperative Care: Remove the protector gently after surgery to avoid dislodging clots or irritating the wound. Dispose of single-use devices properly and sterilize reusable ones according to hospital protocols .
Challenges and Controversies
Cost-Effectiveness: Some studies question the economic viability of wound protectors, particularly in resource-limited settings. A UK-based analysis found no significant cost savings when compared to standard care, though infection rates were lower .
Learning Curve: Inexperienced surgeons may struggle with proper placement, potentially leading to suboptimal outcomes or increased procedural time .
Specialized Cases: In highly contaminated surgeries (e.g., perforated appendicitis), additional antimicrobial measures may be required alongside wound protectors
Surgical wound protectors are indispensable tools in modern operative care, offering tangible benefits in infection prevention, tissue protection, and healing optimization. While challenges like cost and implementation variability exist, ongoing advancements in materials science and technology promise to further refine their efficacy. By adhering to evidence-based guidelines for selection and application, healthcare providers can maximize the clinical and economic advantages of these devices, ultimately improving patient outcomes.